Why "simple" care processes take forever to implement 🐢
Date
May 16, 2024
Category
CareOps
Author
Thomas Vande Casteele
“We just need this simple 2-step workflow”.
Eight months later, it’s still not live. Sound familiar?
As long as AI hasn't turned all of humankind into paperclips, we’ll enjoy experiencing the effects of fallacies and biases at work. It takes a highly self-aware team to not just spot the fallacy but call it out and decide against what feels natural.
The planning fallacy lives where teams underestimate the time and resources needed to complete a project. This can result from over-optimism, insufficient data on potential obstacles, incorrect understanding of reality or pressure from stakeholders to deliver quickly.
When you hear about billion dollar government projects that all of a sudden cost three times as much as budgeted, that’s planning fallacy at play.
Recently, an Awell customer undertook a project that is a beautiful illustration of where it could easily have become an 8 month / triple the budget issue, but didn’t.
This customer, a large US primary care organization, has asked us to keep their secret sauce secret. But there are learnings we can share without spilling the beans.
The simple 2-step care flow involved triggering an automated communication to patient and care team after a recent discharge. The source of the discharge information was a classic ADT-feed, or stream of Admission/Discharge/Transfer events. Provided either directly by hospitals or aggregated by vendors, ADT feeds are the event notification layers of patients going into and out of the hospital. In this case, only discharges were in scope.
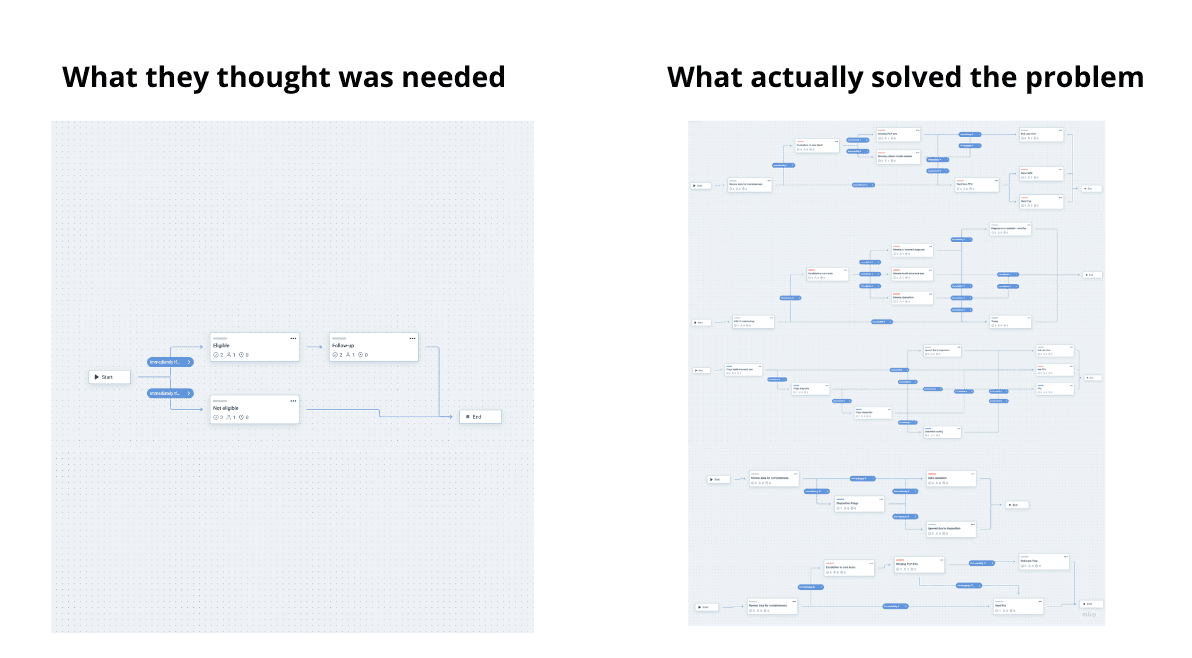
“Within 2 days after discharge event, send message A to patient and message B to care team if discharge diagnosis is one of [X, Y, Z]. Else, route to manual follow-up” is a good verbal representation of the care flow this customer wanted to implement. By and large this was built and operational in a single day with Awell.
But then the plot started thickening.
Overcoming data quality obstacles
Data quality is not always up to standards in healthcare (if you’re reading this and not familiar with healthcare, please notice the sarcasm).
This means the incoming data to trigger the care flow lacked information that was crucial to execute the flow. Missing patient phone numbers. Missing discharge diagnoses. Missing primary care physician name. At first sight, more than 80% of all discharges missed some piece of data.
Instead of only automating 20% of the cases, the team wanted to hunt for the missing data in order to crank up this percentage. This is because every case that could not be automated would end up on the plate of the care team for manual follow-up.
Additional steps were built into the care flow to identify and resolve data gaps. You could argue that this is a responsibility of the data platform or ADT data vendor and the problem should be solved upstream. In any other industry you would be right. But data fragmentation across many systems, in many shapes and types is one of the core reasons why healthcare doesn’t work. If it would have been easy to reconcile data across systems, it would have been done some time ago.
Handling exploding exceptions
Healthcare sometimes feels like exceptions are the rule. That there is no process “trunk” the majority of people flow through and seemingly every case is a unique snowflake. The narrative around precision medicine has exacerbated this perception. The reality is, there is sufficient commonality across humans to create a good amount of standardization.
Nevertheless, this care flow had quite some exceptions. Patients discharged to other locations than their home. Patients who were deceased. Patients with specific health plans that required a different follow-up.
This could again have been a cause for going back to the drawing table. Fortunately, having a CareOps platform means you can make changes to processes and push them out in a matter of hours. So just like with data quality, additional steps and logic were built into the flow to support these exceptions.
Operationalizing the flow
On certain days, the ADT feed would spit out hundreds of discharged patients. Admittedly it’s downright scary to flip an existing modus operandi (“process” would be too much of a word in many cases in healthcare) overnight to a tool that automates most of the work.
Operationalizing the flow meant ramping up the percentage of the population that came through in the ADT feed and were routed to manual handling vs automated handling of the exceptions and escalations. This allowed the team to parallelize the old and the new and perform any additional checks to make sure no patients were falling through the cracks.
As this ramp up took place, additional incremental improvements were done to the flow to make sure it fit the way the care team wanted to work and not the other way around.
The solution: low effort iteration with Awell’s CareOps platform
Taking a bet on working with a highly self-aware and committed team that rows against the current of their own brains is a risky one. Chances are you’ll end up in the 8 months rabbit hole or tripling budget situation yourself - even for “small” changes. And even if you’re lucky in one project, new behavior is hard fought so you’d better prepare for a sequel.
The solution starts by embracing the planning fallacy, not fighting it. Assume you can’t plan it all. You can’t know every intricacy of reality. You can’t perform all checks on the data beforehand. There’s no way you can anticipate all of the exceptions that will rear their heads.
Awell’s customers start small, launch early and iterate their way incrementally to what they need. They realized the only thing that counts is improving over the previous version and doing it relentlessly, and faster than your competitor.
In the last decades, this agile mindset has changed the way software is built - from planning-heavy, waterfall projects that took years to shipping changes continuously. Speed is becoming the new currency in healthcare.
Where DevOps has become mission critical for software teams in the last decade, the next decade will see the same evolution for CareOps. To support this evolution we are building out Awell as the world’s leading CareOps platform to design, implement and continuously improve care flows.
If you want to move quickly on initiatives rather than getting stuck in 8-month delays, reach out and let's discuss how Awell can help iterate your care flows effectively.
Back





